Colonoscopy
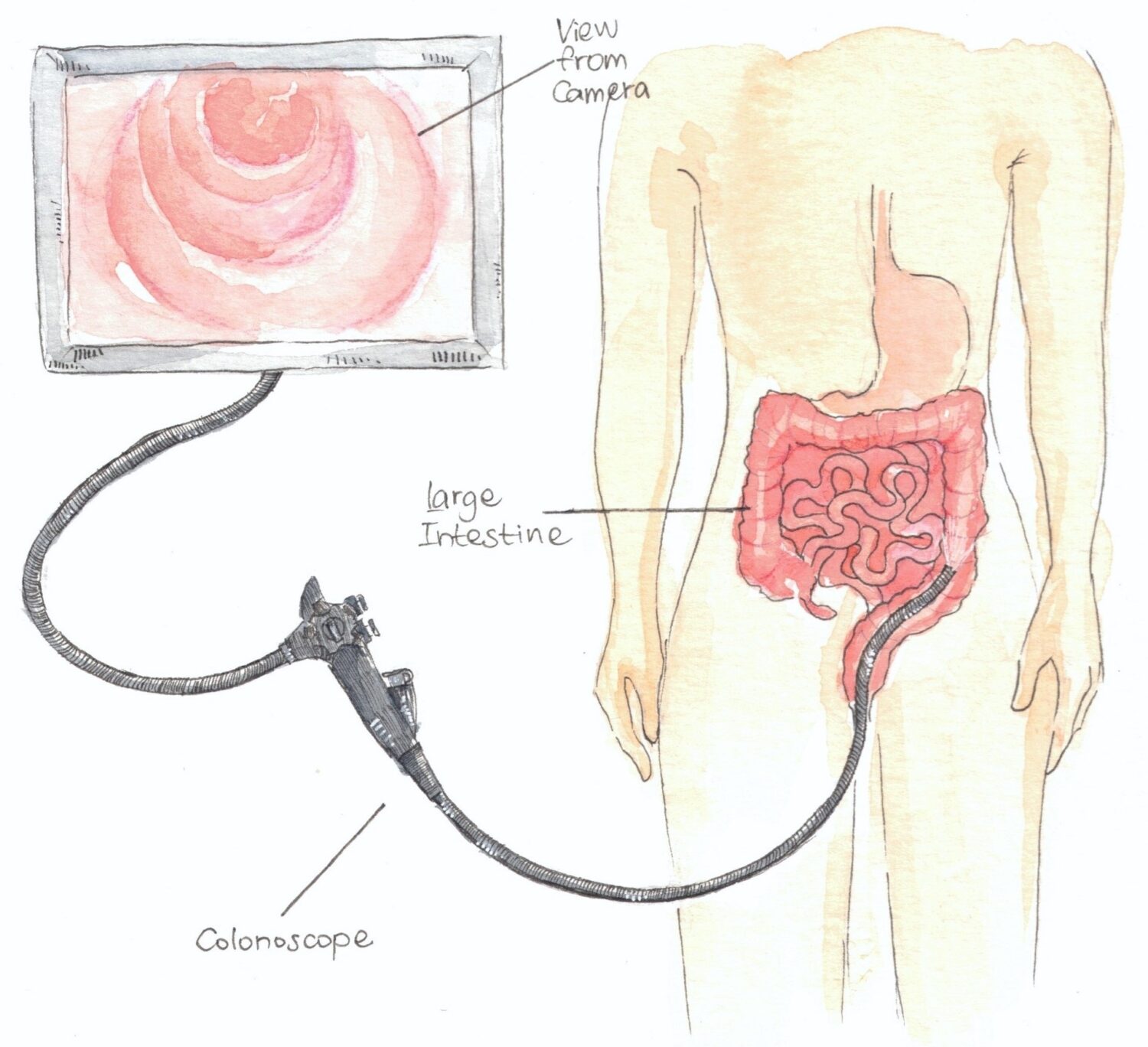
A colonoscopy is an examination of the lower part of the digestive tract, which allows for the inspection of the entire large intestine using a flexible optical instrument (endoscope).
The examination helps to identify the causes of your complaints (such as lower abdominal pain, diarrhea, lower intestinal bleeding) and to find visible pathological changes in the large intestine (such as ulcers, inflammation, tumors).
A colonoscopy is more accurate than noninvasive investigations (X-ray, ultrasound, CT) and allows for the collection of tissue samples (biopsies) as well as procedures such as polypectomy (removal of polyps) during the investigation, which can later be examined under a microscope.
Preparation for the examination
For the colonoscopy to be performed, your large intestine must be clean. Follow the given instructions carefully. To cleanse the bowel, special oral lavage solutions or other laxatives are typically used.
For information about taking your regular medications before the examination preparation, consult the doctor who referred you for the examination.
Medications should be taken 1–3 hours before or at least 1 hour after drinking the bowel cleansing solution. If you are taking blood thinners (e.g. Eliquis (apixaban), Xarelto (rivaroxaban), Lixiana (edoxaban), clopidogrel etc.), make sure to inform your treating physician, since in some cases it is required to pause them before the investigation.
One week before the examination
- Do not eat red beet, tomatoes, fruits, and berries with seeds, or jam.
- Do not eat whole grain products containing seeds (e.g., whole grain bread, bread with seeds).
- Do not take iron or charcoal tablets.
Two days before the examination
- You may only eat low-fiber foods. You can eat broth, pureed soup, juice, jelly, bisquits (without seeds), sausage, mashed potatoes, boiled fish, yogurt without seeds.
- Drink enough fluids (at least 1.5 liters a day).
One day before the examination
- In the morning, you can eat a light, fiber-free meal; do not eat for the rest of the day.
- You may drink throughout the day. Only clear liquids are allowed (e.g., water, tea, juice, broth). Drinks with sweeteners and carbonated drinks are also allowed. Do not drink milk, opaque liquids (red or other strongly colored liquids), liquids with pulp, or alcoholic beverages.
- Prepare the bowel cleansing solution prescribed to you (e.g., Fortrans, Eziclen, Cololyt, Moviprep, Picoprep) according to the manufacturer’s/your healthcare provider’s instructions and based on whether the colonoscopy is scheduled for the morning or afternoon of the following day.
- Bowel movements typically begin 1–2 hours after drinking the first liter of the solution. For better tolerability it can be helpful to drink the solution chilled or to add flavoring, such as lemon juice.
- Since the bowel cleansing solution significantly increases the volume of your bowel contents and cleanses the bowel, we recommend staying near a restroom.
On the day of the examination
On the day of the examination, please do not eat. You may drink clear liquids. At least 2 hours before the examination, drinking is also not allowed.
Performing the examination
Before the examination, you will need to sign a consent form.
Wear clothes with separate upper and lower parts, as you will be given disposable shorts to wear to ensure privacy during the examination.
During the examination, you will lie on one side with your knees bent towards your chest or on your back. The colonoscope is inserted into the large intestine through the anus, and by expanding the colon with water and air, it is possible to detect pathological changes.
Due to the stretching of the bowel with air, you may feel mild abdominal pain and a feeling of fullness, but these symptoms usually subside within a few hours.
The examination lasts about 30-60 minutes.
Rarely low dosages of mild anesthetics can be used intravenously (typically unnecessary), which may cause lightheadedness. In this case you cannot drive for 24 hours after the examination.
After the examination
You may eat and drink immediately unless otherwise instructed by your doctor.
The results of the examination will be written by the doctor who performed the colonoscopy immediately after the procedure. The results will be sent electronically to your treating physician.
Possible complications
Colonoscopy is a safe examination method with complications occurring rarely:
- Bleeding following biopsy/polyp removal is typically minimal, does not require blood transfusions or surgical treatment and is usually treated during the examination.
- Perforation of the colon wall is very rare but may require surgical treatment.
If you experience fever, severe abdominal pain, or bleeding after the examination, immediately contact your family doctor or, if you are hospitalized, the on-duty nurse or your treating physician.
Endoscopy Center
Tartu University Hospital, Internal Medicine Clinic
L. Puusepa 8, Building J, 3rd Floor
To cancel your appointment, call 731 9099 (Mon-Fri 07:30-18:00) or submit your request on the hospital’s website under the “For Patients” section.
Compiled by: Marika Kukk, head nurse of the gastroenterology department
Illustrated by: dr Ana Botchorishvili
Translated by: Kirke Naarits, RN
2023